|
 Instructions
Instructions
 Take Another Course
Take Another Course
 Post-Test
Post-Test
|
Lower Extremity Wound - Venous
Stasis Wounds
|
We are going to discuss 3 different types of lower
extremity wounds--Venous, Arterial and Diabetic. It
is very important to differentiate between them
because their treatment plans can be very different.
We will start with Venous Stasis Wounds.
As you know....these wounds are caused by veins that
are not pumping well....causing venous
insufficiency.
These wounds:
*are located in the “gaiter” area, and
*have irregular borders. They
*are often shallow, and
*have a red/yellow base, and
*often have a large amount of drainage.
•The
patient will have normal pulses unless they have
arterial diagnosis as well.
•And
they may have some pain that is often worse with
legs dependent.
* ABI normal |

 |
Treatment for Venous
Stasis Wounds
* Always
includes some type of Compression:
•Unna boots
•2, 3, 4 layer
compression systems
•Compression
ace type wraps that give 30-40 mm pressure
•Tubi grip
•Topical
treatment--used under the compression
•Any advanced
wound care product that is appropriate for the
wound--alginate and foam are the most common
•Patient should
be taught leg elevation
|
 |
Lower Extremity Wounds - Arterial Wounds
•* located most
often on the feet/toes/ occasionally on the legs
•* pulses
reduced or absent
•* abnormal ABI--below
0.8
•* “cookie
cutter” appearance
•* often have
necrotic tissue
•* are very
painful
•* legs feel
better in a dependent position
•* little edema
•* lack of hair
on feet and toes
•*vascular
assessment
•* if needed
and medically possible
•* goals are to
keep clean and uninfected
•* control the
pain
•* hyperbaric
oxygen may be an option
Topical Care can include appropriate advanced wound
care treatment |
 |
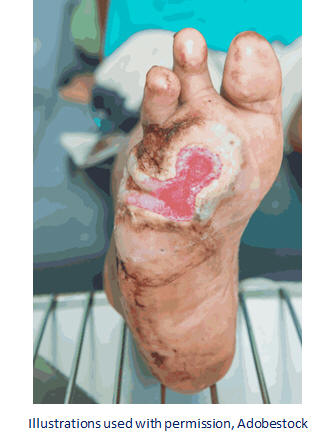
| Diabetic
Wounds
And now Diabetic Wounds: These are caused by
diabetic neuropathy.
These patients often have a “LOSS of Protective
Sensation” to the feet.
They may have many foot deformities, such as hammer
toes, claw toes, bunions, callous, and Charcot foot
(charcot foot is a foot where the structural
integrity of the foot is lost by boney changes and
inflamation).
Diabetic wounds are often found on the plantar area
of the foot and over the metatarsal heads. These
wounds often have little pain, which can be a
problem because the patient may not even recognize
that they have the wound, or they may not realize
the severity of the wound.
These wounds can build up a callous very
easily--often making the clinician think the wound
is getting smaller, but really the callous is hiding
the wound below. These wounds need to be debrided on
a regular basis—generally every 1-3 weeks. |
 |
|
Treatment for the Diabetic Foot
Wounds
These wounds MUST be offloaded 24/7--this means
special shoes, boots, contact casts, special foam
padding, wheelchairs, crutches, or some other means.
Topical treatments include: alginates with silver,
silver gels, collagen products and other advanced
wound care products.
Negative wound therapy is also often a good choice
for these wounds…(it also keeps them off their feet,
which is a nice side benefit).
Remember to teach all patients diabetic foot care.
This may save their foot.
Teach patients that the first sign of an infection
may not be an elevated temperature, but an elevated
blood sugar. BS needs to be at normal levels for
wound healing.
So, to sum up here, we have briefly covered three
different types of lower extremity wounds. Remember
that your patient may have just one of these, or
could have mixed disease...making the treatment plan
and healing much more difficult.
|
|
|